Menu
Why CHOLINE CAN Help YOUR BABY's BRAIN DeVELOPMENT
Targeting treatments to genes
Genetic research in schizophrenia points to a complex set of risks, transmitted through families and involving many genes, including those responsible for the earliest stages of brain development before birth. One of the first genes identified as causing a specific brain deficit in schizophrenia is called CHRNA7, which makes a key brain receptor--the alpha7-nicotinic cholinergic receptor. Receptors are proteins on the surface of nerve cells that receive chemical signals from other nerve cells, enabling these cells to communicate with each other. This receptor is normally activated by a brain chemical called acetylcholine, but as its name implies, nicotine can also activate it.
Because of abnormalities in the CHRNA7 gene, some limited to a single DNA basepair, the number of receptors needed for normal functioning is reduced in the brains of many people with schizophrenia. Patients lose the ability to filter out noise around them and then frequently misperceive voices that become part of their hallucinations and delusions.
Alpha7-nicotinic receptor levels peak in the fetal brain; they then diminish after birth to adult levels. Intervention targeted to CHRNA7 therefore is likely more effective before birth, when the gene is most active and the brain is undergoing its most critical period of development. At this time of life, CHRNA7’s receptors are key to helping other nerve cells mature, including nerve cells that inhibit excess response to noise. Acetylcholine does not reach these alpha7-nicotinic receptors until just before birth. Throughout most of pregnancy, choline surrounding the baby activates the receptors.
Intervening in pregnancy
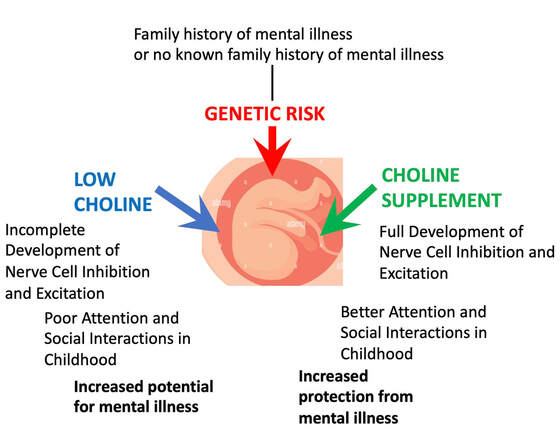
It is not possible to test fetuses to see if they have any of the hundreds of gene variants associated with schizophrenia, even within one gene like CHRNA7. Treatment must be safe for all pregnant women and their babies, including those who have no risk for illness. Choline is such a treatment. The unique opportunity in pregnancy is that increasing the mother’s choline levels by supplementing choline in her diet activates the fetus’s alpha7-nicotinic receptors and promotes normal brain development even in those at risk for mental illness. (Figure 1).
This supplement approach to prevention is akin to the now widespread use of folic acid supplements during pregnancy to prevent spina bifida. Although spina bifida is rare, folic acid in large amounts is offered to all pregnant women. Even in babies with genetic risk for spina bifida, the folic acid supplement induces the spinal cord to fuse normally and permanently. A second similarity with choline is that folic acid is also effective for a wide variety of developmental defects, from cleft palate to microcephaly. CHRNA7 mutations, active in the development of schizophrenia, are also found in autism spectrum and attention deficit disorder.
Both folic acid and choline are naturally found in food, and both can be safely given to women even if they have no known risk factors for their babies’ development. The possible impact of even partial prevention on the global burden of mental illness could be quite substantial.
Genetic research in schizophrenia points to a complex set of risks, transmitted through families and involving many genes, including those responsible for the earliest stages of brain development before birth. One of the first genes identified as causing a specific brain deficit in schizophrenia is called CHRNA7, which makes a key brain receptor--the alpha7-nicotinic cholinergic receptor. Receptors are proteins on the surface of nerve cells that receive chemical signals from other nerve cells, enabling these cells to communicate with each other. This receptor is normally activated by a brain chemical called acetylcholine, but as its name implies, nicotine can also activate it.
Because of abnormalities in the CHRNA7 gene, some limited to a single DNA basepair, the number of receptors needed for normal functioning is reduced in the brains of many people with schizophrenia. Patients lose the ability to filter out noise around them and then frequently misperceive voices that become part of their hallucinations and delusions.
Alpha7-nicotinic receptor levels peak in the fetal brain; they then diminish after birth to adult levels. Intervention targeted to CHRNA7 therefore is likely more effective before birth, when the gene is most active and the brain is undergoing its most critical period of development. At this time of life, CHRNA7’s receptors are key to helping other nerve cells mature, including nerve cells that inhibit excess response to noise. Acetylcholine does not reach these alpha7-nicotinic receptors until just before birth. Throughout most of pregnancy, choline surrounding the baby activates the receptors.
Intervening in pregnancy
It is not possible to test fetuses to see if they have any of the hundreds of gene variants associated with schizophrenia, even within one gene like CHRNA7. Treatment must be safe for all pregnant women and their babies, including those who have no risk for illness. Choline is such a treatment. The unique opportunity in pregnancy is that increasing the mother’s choline levels by supplementing choline in her diet activates the fetus’s alpha7-nicotinic receptors and promotes normal brain development even in those at risk for mental illness. (Figure 1).
This supplement approach to prevention is akin to the now widespread use of folic acid supplements during pregnancy to prevent spina bifida. Although spina bifida is rare, folic acid in large amounts is offered to all pregnant women. Even in babies with genetic risk for spina bifida, the folic acid supplement induces the spinal cord to fuse normally and permanently. A second similarity with choline is that folic acid is also effective for a wide variety of developmental defects, from cleft palate to microcephaly. CHRNA7 mutations, active in the development of schizophrenia, are also found in autism spectrum and attention deficit disorder.
Both folic acid and choline are naturally found in food, and both can be safely given to women even if they have no known risk factors for their babies’ development. The possible impact of even partial prevention on the global burden of mental illness could be quite substantial.
Genetic risk for the baby’s future mental illness may be present regardless of whether or not the parents have family histories of mental illness. Some genes, notably CHRNA7, can have problematic variations in their DNA that are associated with mental illness. These variants lead to fewer CHRNA7 receptors and poorer development of nerve cell inhibition and excitation. These nerve cell problems are first seen as poor attention and social interactions in early childhood. Later in life poor nerve cell development increases the risk for mental illnesses. Choline supplements can mitigate some of the developmental problems from genetic risk, promote better development of inhibition and excitation, and hopefully result in a healthier child.
Proudly powered by Weebly